Radiation Oncology
About Radiation Oncology at AMC
Radiation Oncology, a subspecialty of Oncology, uses radiation therapy to complement surgery and systemic treatments (chemotherapy and immunotherapy) in the treatment and eradication of tumors. Although some tumors may be best treated with only one of these modalities, many tumors, both malignant and benign, are best treated with a combination of these modalities. AMC’s collaborative and comprehensive Oncology teams will make sure your pet receives the best oncology care possible.
What types of tumors can be treated with radiation?
All tumors can potentially be treated with radiation therapy, but not all tumors respond the same to radiation and recommended treatments will, therefore, depend on the location of the tumor, the type of tumor, the anticipated behavior of the tumor and prognosis, the overall health status of the patient, and other factors.
Tumors frequently referred for radiation therapy include:
- Skin tumors and soft tissue tumors of the limbs and trunk (soft tissue sarcomas, mast cell tumors, carcinomas, melanomas)
- Bone tumors (of limbs, skull, spine, and pelvis)
- Joint tumors
- Nasal and oral tumors (sarcomas, carcinomas, melanomas, odontogenic tumors, lymphoma, tonsillar, and tongue tumors)
- Tumors of the larynx, pharynx, and trachea
- Brain tumors/spinal cord tumors
- Periocular and facial tumors
- Ear tumors
- Thyroid tumors
- Anal sac adenocarcinoma
- Anal/rectal tumor
- Bladder/prostate and urethral tumors
- Heart base and mediastinal tumors (thymoma, chemodectoma, ectopic thyroid, lymphoma, and other less common)
- Non-resectable lung masses and other thoracic tumors
- Non-surgical abdominal/pelvic tumors
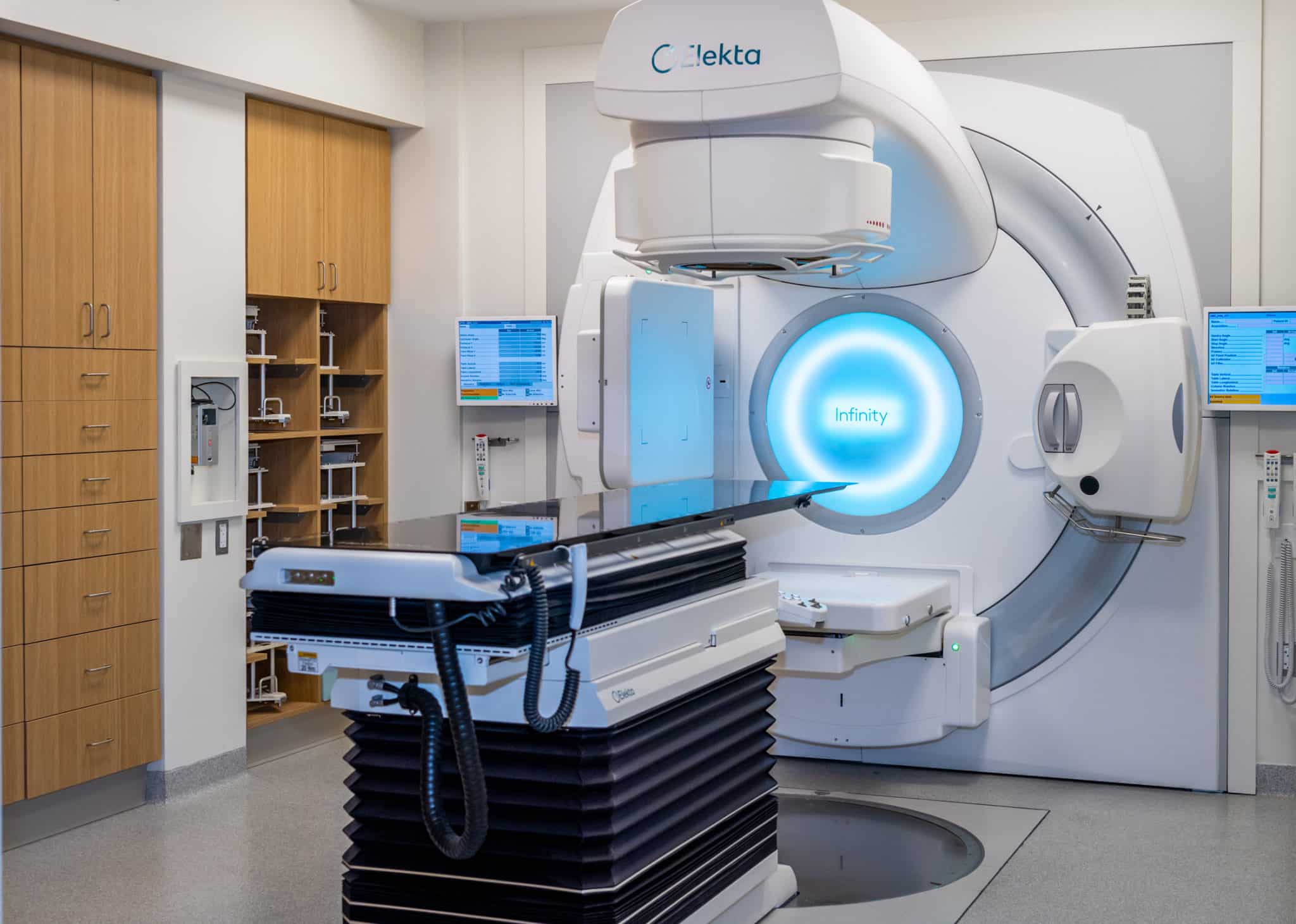
The Elekta Infinity HD Linear Accelerator
In October 2022, we introduced a new, state-of-the-art radiation therapy machine at AMC: the Elekta Infinity HD linear accelerator (LINAC). With this technology, we can treat any tumor in any part of the body better than we’ve ever been able to before.
Benefits of the Elekta Infinity HD LINAC
Precise radiation delivery for even the smallest patients with on-board CT scan verification linked to a robotic treatment table capable of adjusting patient position with full direction of freedom to sub-millimeter and sub-degree accuracy.
Efficient treatment delivery helping to reduce side effects and improve time of delivery using sophisticated technology to:
- Enhance modulation of dose administration using the fastest and most precise multi-leaf collimator available in linear accelerators. This allows superior treatment planning for all IMRT, VMAT, Stereotactic and radiosurgery (SRT, SBRT, and SRS) radiation.
- Markedly increased dose rate capability leading to faster treatment delivery, reducing anesthesia time for our patients.
Our Team
DVM, MVSc, DACVR (RO)
Radiation Oncology Residency Program Director